Vector-Borne Diseases US: 25% Increase by 2025 Health Risk
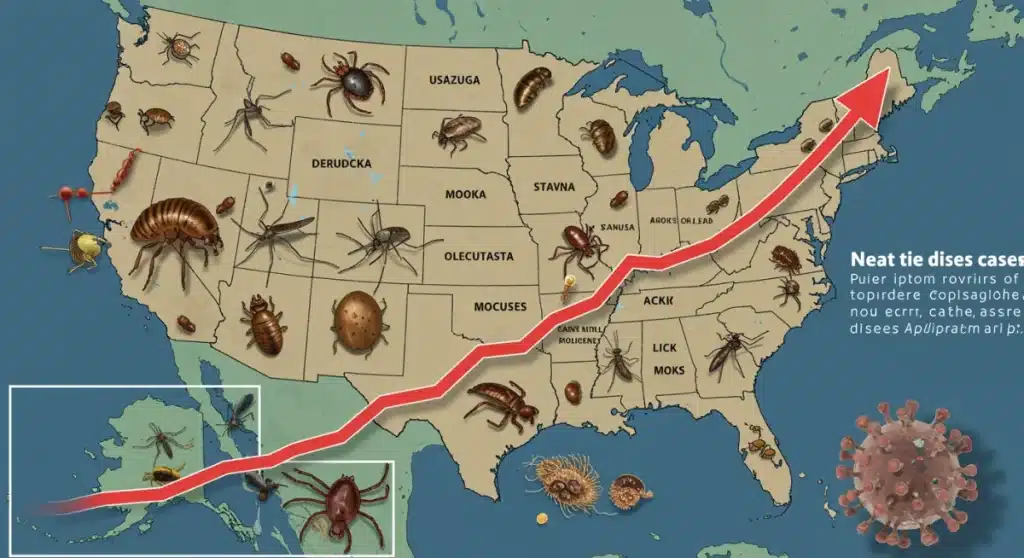
Experts project a 25% surge in vector-borne diseases across the US by 2025, driven by climate change and ecological shifts. This report details the health risks, contributing factors, and urgent strategies needed for prevention and public health.
The alarm is sounding across the United States: a projected vector-borne disease increase of 25% by 2025 is now a critical public health concern. This imminent threat, highlighted by recent analyses, demands immediate attention from policymakers, healthcare providers, and the public. Understanding the scope and drivers behind this surge is crucial for effective mitigation.
The Looming Threat: A 25% Increase in Vector-Borne Diseases
New data and expert consensus point to an unsettling reality: the United States is on track to experience a significant rise in vector-borne diseases. This 25% surge by 2025 is not merely a statistical projection but a warning based on observable trends and environmental shifts. Diseases transmitted by mosquitoes, ticks, and fleas are expanding their geographic reach and incidence, putting millions more Americans at risk.
This projected increase signifies a profound challenge to public health infrastructure, requiring proactive measures rather than reactive responses. The impact extends beyond individual illness, potentially straining healthcare systems, affecting local economies, and altering lifestyle patterns in affected regions. The urgency to address this trend is paramount, as the window for effective intervention narrows with each passing season.
Key Drivers of the Increase
- Climate Change: Warmer temperatures and altered precipitation patterns are extending vector breeding seasons and expanding their habitats, allowing them to thrive in new areas.
- Land Use Changes: Deforestation and urbanization can bring vectors into closer contact with human populations, increasing transmission opportunities.
- Global Travel and Trade: The movement of people and goods facilitates the introduction of new vector species and pathogens into previously unaffected regions.
- Ecosystem Disruption: Changes in biodiversity can impact natural predators of vectors, leading to increased vector populations.
The convergence of these factors creates a complex web that favors the spread of diseases like Lyme disease, West Nile virus, Zika, and dengue. Public health officials are now working to refine surveillance strategies and prepare for the anticipated rise in cases, emphasizing the need for a multi-faceted approach.
Climate Change: The Primary Catalyst for Disease Expansion
Climate change stands out as the most significant factor fueling the projected vector-borne disease increase. Rising global temperatures directly influence the life cycles and geographical distribution of disease-carrying insects and arachnids. This environmental shift is creating new breeding grounds and extending transmission seasons, fundamentally altering disease epidemiology across the US.
For instance, warmer winters mean fewer vectors die off, leading to larger populations in the spring. Increased rainfall in some areas creates more stagnant water bodies, ideal for mosquito breeding. Conversely, droughts followed by heavy rains can also create breeding pockets. These changes are not uniform but create a mosaic of new risks across different regions, from the temperate Northeast to the arid Southwest.
Impact on Vector Distribution and Activity
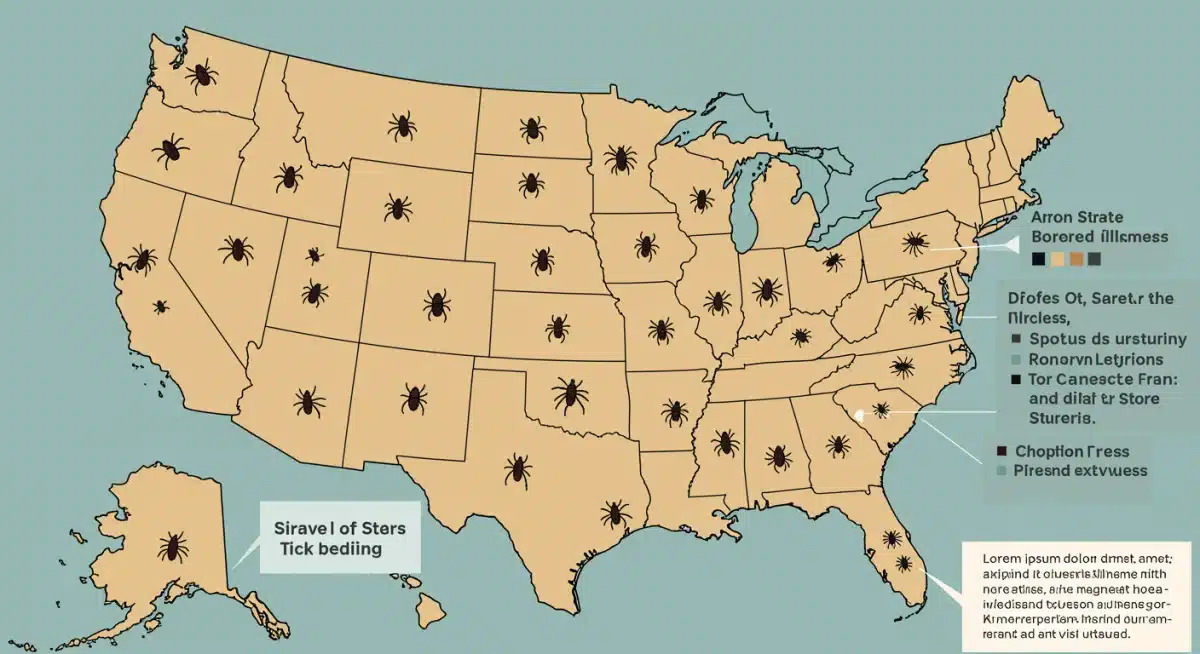
The geographic spread of vectors is undeniable. Mosquitoes carrying West Nile virus are now found in areas where they were historically rare, and the range of tick species responsible for Lyme disease continues to push northward and westward. This expansion means communities previously unaccustomed to these threats must now adapt their public health strategies and personal protective measures.
Moreover, the activity period of these vectors is lengthening. Ticks are active earlier in the spring and later into the fall, increasing the window for human exposure. Mosquitoes can remain active for more months of the year, amplifying the risk of outbreaks. This extended activity directly correlates with the projected vector-borne disease increase, demanding year-round vigilance.
The scientific consensus is clear: climate change is not a distant threat but a present reality actively shaping the landscape of infectious diseases. Addressing this underlying cause is crucial for any long-term strategy to control vector-borne illnesses. Without significant climate action, the fight against these diseases will remain an uphill battle.
Understanding the Major Vector-Borne Threats in the US
As the US braces for a 25% vector-borne disease increase by 2025, understanding the specific threats posed by different vectors is paramount. While numerous pathogens can be transmitted, a few stand out due to their prevalence, severity, and projected expansion. These include diseases transmitted by ticks, mosquitoes, and to a lesser extent, fleas.
Lyme disease, transmitted by blacklegged ticks, remains the most common vector-borne illness in the US, primarily affecting the Northeast and Midwest. However, its geographic footprint is steadily growing. Other tick-borne diseases like anaplasmosis, babesiosis, and Rocky Mountain spotted fever also present significant health challenges, with varying regional concentrations.
Mosquito-Borne Illnesses on the Rise
Mosquitoes are responsible for a range of illnesses, with West Nile virus being the most widespread in the continental US. While often mild, it can cause severe neurological disease. Other mosquito-borne threats include Eastern Equine Encephalitis (EEE), a rare but deadly disease, and dengue and Zika viruses, which are becoming more prevalent in US territories and increasingly reported in southern states due to local transmission.
The expansion of Aedes mosquito species, particularly Aedes aegypti and Aedes albopictus, is a critical concern. These invasive species are highly efficient vectors for dengue, Zika, and chikungunya, posing a risk for future outbreaks in urban and suburban areas previously unaffected. The projected vector-borne disease increase is heavily influenced by the adaptability and spread of these mosquito types.
Beyond ticks and mosquitoes, flea-borne typhus and even plague, though rare, are also present in certain regions of the US. Public health surveillance systems are actively monitoring these threats, but increased community awareness and preventative actions are essential to curb their spread. Education on identifying vectors and symptoms is a key component of public safety.
Public Health Preparedness and Response Strategies
In response to the anticipated 25% vector-borne disease increase, public health agencies across the US are intensifying their preparedness and response strategies. This involves a multi-pronged approach that integrates surveillance, prevention, community engagement, and rapid intervention to mitigate the impact of rising caseloads. The goal is to build resilience against these evolving threats.
Enhanced surveillance systems are crucial for tracking vector populations and disease incidence. This includes monitoring climate data, conducting field surveys for ticks and mosquitoes, and promptly reporting human cases. Early detection allows for targeted interventions, such as pesticide applications or public awareness campaigns in high-risk areas. Investing in diagnostic capabilities is also vital for quick and accurate identification of pathogens.

Community-Level Interventions
- Vector Control Programs: Implementing integrated pest management strategies, including source reduction (eliminating standing water), larvicides, and adulticides where appropriate.
- Public Education Campaigns: Informing residents about personal protective measures, such as using repellents, wearing protective clothing, and performing tick checks.
- Habitat Modification: Encouraging landscape changes that reduce vector breeding sites around homes and in public spaces.
- Early Warning Systems: Developing and communicating alerts based on surveillance data to inform communities of elevated risk periods.
Effective public health response also requires robust healthcare system capacity. Hospitals and clinics must be prepared to diagnose and treat a wider array of vector-borne illnesses, ensuring healthcare professionals are educated on the latest clinical guidance. Collaboration between local, state, and federal agencies is essential for a coordinated and effective response to this growing public health challenge.
Personal Protection: Reducing Your Risk Amidst Rising Threats
With a projected 25% vector-borne disease increase across the US by 2025, personal protection measures are more critical than ever. While public health agencies implement large-scale interventions, individual actions play a significant role in reducing exposure and preventing illness. Empowering yourself with knowledge and adopting preventative habits can drastically lower your risk.
The first line of defense involves avoiding vector habitats whenever possible. This means exercising caution in wooded areas, tall grass, and stagnant water bodies, especially during peak vector activity times. When outdoor activities are unavoidable, proper clothing and repellents become indispensable tools in your arsenal against bites and stings.
Essential Personal Protective Strategies
- Use EPA-Registered Repellents: Apply repellents containing DEET, picaridin, IR3535, oil of lemon eucalyptus (OLE), para-menthane-diol (PMD), or 2-undecanone to exposed skin and clothing.
- Wear Protective Clothing: When in tick-prone areas, wear long-sleeved shirts, long pants tucked into socks, and light-colored clothing to spot ticks more easily.
- Perform Regular Tick Checks: After spending time outdoors, thoroughly check your body, clothing, and pets for ticks. Pay close attention to hair, ears, armpits, navel, and behind the knees.
- Eliminate Standing Water: Regularly empty and clean items that can collect water around your home, such as birdbaths, pet bowls, flowerpots, and gutters, to prevent mosquito breeding.
Promptly removing attached ticks is vital, as the risk of disease transmission increases with the duration of attachment. Use fine-tipped tweezers to grasp the tick as close to the skin’s surface as possible and pull upward with steady, even pressure. Following these simple yet effective guidelines can significantly reduce your vulnerability to the impending vector-borne disease increase and protect your health.
The Economic and Social Impact of Increased Disease Burden
The anticipated 25% vector-borne disease increase in the US by 2025 extends far beyond individual health consequences, posing substantial economic and social challenges. The rising incidence of illnesses like Lyme disease, West Nile virus, and dengue will place an immense burden on healthcare systems, productivity, and community well-being across affected regions.
Economically, the direct costs include increased medical expenditures for diagnosis, treatment, and long-term care for chronic conditions resulting from severe infections. This also translates to lost productivity due to illness-related absenteeism from work and school, impacting local economies and national GDP. Furthermore, tourism and outdoor recreation industries in affected areas may suffer as people become more hesitant to engage in activities perceived as high-risk.
Societal Repercussions and Quality of Life
Socially, the rising disease burden can lead to increased anxiety and fear within communities, particularly in areas experiencing new or intensified outbreaks. The chronic nature of some vector-borne illnesses can significantly diminish the quality of life for individuals, leading to persistent pain, fatigue, and neurological issues that affect daily functioning and mental health. This places additional demands on social support systems and public health resources.
Moreover, the need for enhanced vector control measures often comes with its own costs and potential environmental considerations. Decisions about pesticide use, for example, must balance public health protection with ecological impact. The complexity of these challenges underscores the need for comprehensive and sustainable solutions to manage the projected vector-borne disease increase effectively, ensuring both human health and environmental integrity.
Future Outlook: Innovations and Collaborative Solutions
Addressing the projected 25% vector-borne disease increase by 2025 requires not only current mitigation strategies but also foresight into future innovations and strengthened collaborative efforts. Researchers, public health officials, and technology developers are actively exploring new frontiers to combat these evolving threats, from novel diagnostic tools to advanced vector control methods.
One promising area is the development of more effective vaccines against diseases like Lyme and dengue. While some vaccines exist, continuous research is vital to improve their efficacy and broaden their availability. Additionally, advancements in gene-editing technologies, such as CRISPR, hold potential for creating mosquitoes that are resistant to carrying certain viruses or that have reduced reproductive capacities, offering a targeted approach to vector control.
The Role of Data and Technology
Big data analytics and artificial intelligence are revolutionizing disease surveillance. Predictive modeling can forecast outbreak risks based on environmental factors, allowing for pre-emptive interventions. Satellite imagery and drone technology can identify potential breeding sites more efficiently, guiding vector control efforts. These technological integrations are crucial for a proactive stance against the vector-borne disease increase.
Ultimately, a truly effective response hinges on interdisciplinary collaboration. This involves partnerships between government agencies, academic institutions, non-profit organizations, and international bodies. Sharing data, research findings, and best practices across borders and sectors will accelerate the development and implementation of sustainable solutions, ensuring a more resilient future against vector-borne threats.
Key Point |
Brief Description > |
|---|---|
Projected Increase |
A 25% rise in vector-borne diseases across the US is anticipated by 2025. |
Primary Driver |
Climate change is extending vector habitats and breeding seasons, intensifying risks. |
Major Threats |
Lyme disease, West Nile, Zika, and dengue are key concerns due to expanding ranges. |
Mitigation |
Enhanced surveillance, personal protection, and innovative vector control are crucial. |
Frequently Asked Questions About Vector-Borne Disease Increase
The primary drivers are climate change, leading to warmer temperatures and altered precipitation patterns that expand vector habitats and lengthen breeding seasons. Land use changes, global travel, and ecosystem disruptions also contribute significantly to this alarming trend across the US.
Lyme disease (tick-borne) and West Nile virus (mosquito-borne) are currently widespread. However, diseases like dengue, Zika, and chikungunya are becoming increasingly concerning, particularly in southern states and US territories, due to the expansion of their mosquito vectors.
Key measures include using EPA-registered insect repellents, wearing protective clothing in high-risk areas, performing regular tick checks after outdoor activities, and eliminating standing water around homes to prevent mosquito breeding. These actions significantly reduce personal exposure.
Public health agencies are enhancing surveillance systems for vectors and diseases, implementing community-level vector control programs, and launching public education campaigns. They are also improving diagnostic capabilities and coordinating responses across local, state, and federal levels.
Beyond individual health, the increase will strain healthcare systems, lead to significant economic costs from medical expenses and lost productivity, and potentially impact tourism and outdoor recreation. It also raises societal anxiety and diminishes the quality of life for affected communities.
What Happens Next
The projected 25% vector-borne disease increase by 2025 is not a distant threat but an imminent reality demanding sustained attention. As climate patterns continue to shift, the geographic spread and intensity of these diseases will evolve. Public health officials and researchers are working to refine predictive models and develop innovative control methods, but the effectiveness of these efforts will largely depend on continued funding, inter-agency collaboration, and robust public engagement. Monitoring regional outbreak data and adhering to expert guidance will be crucial for communities and individuals alike in navigating this evolving health landscape.