Climate Change’s Respiratory Toll: 10% Rise in US Cities by 2025
The escalating human cost of climate change is starkly evident with projections indicating a 10% rise in respiratory illnesses in US cities by 2025, demanding immediate attention to public health and environmental policies.
Climate change respiratory illnesses are emerging as a critical public health crisis, with new data projecting a sobering 10% rise in respiratory illnesses across major US cities by 2025. This alarming forecast underscores the direct and intensifying impact of environmental shifts on human health, demanding immediate and coordinated action.
The Alarming Rise in Respiratory Illnesses
Recent scientific analyses and public health reports reveal a clear and concerning trend: climate change is a significant accelerant for respiratory ailments. This isn’t a future threat; it’s a current reality with projections showing a tangible increase in cases within the next two years. The rise is attributed to a confluence of factors directly linked to a warming planet, affecting air quality and human vulnerability.
The implications are far-reaching, impacting not just individual health but also healthcare systems, economic productivity, and overall urban resilience. Understanding the mechanisms driving this increase is crucial for developing effective mitigation and adaptation strategies.
Mechanisms Linking Climate Change to Respiratory Health
The connection between a changing climate and respiratory health is multifaceted, involving several interconnected environmental and biological processes. Rising temperatures, altered precipitation patterns, and increased frequency of extreme weather events all play a role in exacerbating respiratory conditions. These factors create a more hostile environment for respiratory well-being, particularly in dense urban areas.
As global temperatures continue to climb, the air we breathe becomes a greater threat. Pollutants are trapped closer to the ground, and allergic seasons are extended, directly contributing to a surge in respiratory complications.
Air Quality Degradation
- Increased Ozone Levels: Warmer temperatures accelerate the formation of ground-level ozone, a potent respiratory irritant.
- Particulate Matter: Droughts and wildfires, intensified by climate change, release fine particulate matter into the atmosphere, which can penetrate deep into the lungs.
- Allergen Proliferation: Higher CO2 levels and warmer temperatures extend pollen seasons and increase pollen potency, impacting allergy and asthma sufferers.
These atmospheric changes create a toxic cocktail for urban populations, leading to conditions ranging from mild irritation to severe, life-threatening respiratory events. The elderly, children, and individuals with pre-existing conditions are particularly vulnerable to these environmental stressors.
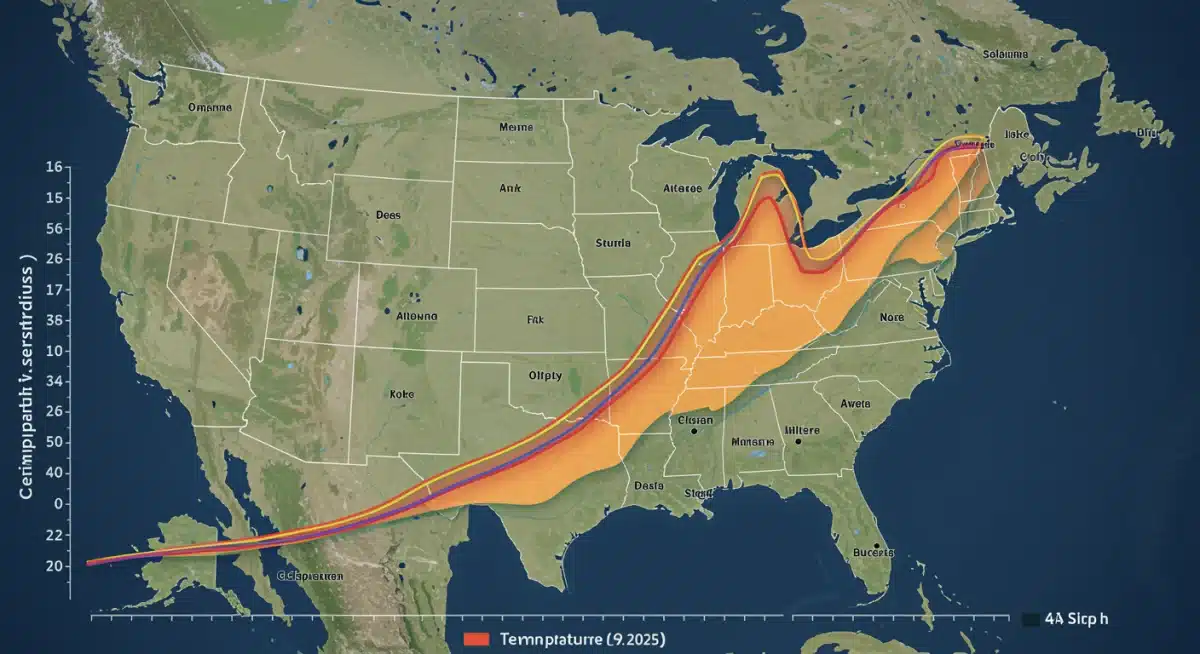
Urban Hotspots: Why US Cities Are at High Risk
US cities, with their dense populations and often compromised air quality, are particularly susceptible to the projected surge in respiratory illnesses. Urban heat islands, combined with existing pollution sources, create an amplified effect that disproportionately impacts city dwellers. This makes cities critical focal points for intervention and public health strategies.
The infrastructure and demographic profiles of many US cities also present unique challenges. Older buildings may lack proper ventilation, and lower-income communities often reside near industrial areas, compounding their exposure to pollutants.
Vulnerability Factors in Urban Environments
- Urban Heat Island Effect: Cities retain more heat, leading to higher temperatures and increased ozone formation.
- Concentrated Populations: A higher density of people means more individuals exposed to degraded air quality and allergens.
- Existing Pollution Burden: Many cities already struggle with industrial and vehicular emissions, which are exacerbated by climate change impacts.
The combination of these factors creates a high-risk environment where even small changes in climate can lead to significant public health consequences. Local governments and health authorities are increasingly under pressure to address these growing concerns.
The Economic and Social Burden of Rising Illnesses
Beyond the immediate health impacts, a 10% rise in respiratory illnesses by 2025 carries substantial economic and social costs. Increased healthcare expenditures, lost productivity due to illness, and a diminished quality of life for affected individuals represent a significant burden on society. This projected increase is not just a health crisis but an economic and social challenge that requires robust policy responses.
Hospitals and clinics face increased patient loads, straining resources and personnel. Businesses experience higher absenteeism, impacting economic output. The ripple effects extend to educational institutions, with children missing school due to illness.
Key Socio-Economic Impacts
- Healthcare System Strain: Increased hospitalizations, emergency room visits, and demand for specialized respiratory care.
- Productivity Loss: Sick days, reduced work capacity, and premature mortality affect economic output.
- Educational Disruptions: Children’s school attendance and learning abilities are compromised by chronic respiratory issues.
These costs are often borne disproportionately by vulnerable communities, widening existing health and economic disparities. Addressing climate change respiratory illnesses is therefore not just a health imperative but a matter of social equity.

Mitigation and Adaptation Strategies for US Cities
Addressing the projected rise in respiratory illnesses requires a dual approach: mitigating climate change to reduce its root causes and adapting urban environments to protect public health. These strategies must be integrated, comprehensive, and implemented with urgency to safeguard city residents.
Efforts range from global policy changes to local community initiatives. Investing in renewable energy, improving urban planning, and enhancing public health surveillance are all vital components of a resilient response to the health impacts of climate change.
Essential Actions for Urban Resilience
- Green Infrastructure Development: Planting more trees and creating green spaces to reduce urban heat and filter air.
- Air Quality Monitoring and Warning Systems: Implementing advanced systems to alert residents to high pollution days.
- Public Health Campaigns: Educating the public on protective measures and early symptom recognition for respiratory issues.
By combining these strategies, cities can build greater resilience against the health threats posed by climate change, protecting their populations from the increasing burden of respiratory illnesses. Proactive measures are essential to avert the worst outcomes.
The Path Forward: Policy and Public Engagement
The projected 10% rise in respiratory illnesses demands a robust policy framework and active public engagement. Governments at all levels, from federal to municipal, must prioritize policies that aggressively reduce greenhouse gas emissions and invest in climate-resilient public health infrastructure. Public awareness and individual actions are also critical components of this collective effort.
Engaging communities, particularly those most at risk, is paramount. Empowering citizens with information and resources can foster a sense of shared responsibility and drive grassroots change. The focus must be on creating sustainable, healthy urban environments.
Key Policy and Engagement Areas
- Stricter Emission Standards: Implementing and enforcing regulations to curb industrial and vehicular pollution.
- Investment in Renewable Energy: Transitioning away from fossil fuels to cleaner energy sources.
- Community Health Programs: Developing targeted programs to support vulnerable populations and provide access to care.
Ultimately, addressing the human cost of climate change respiratory illnesses requires a coordinated, multi-sectoral approach that integrates environmental protection with public health initiatives. The urgency of the 2025 projection serves as a stark reminder of the need for immediate and decisive action.
Key Point > | Brief Description > |
|---|---|
Projected Increase > |
10% rise in respiratory illnesses in US cities by 2025 due to climate change. > |
Driving Factors > |
Degraded air quality, increased allergens, and extreme weather events linked to global warming. > |
Urban Vulnerability > |
Dense populations, urban heat islands, and existing pollution burdens amplify risks in cities. > |
Call to Action > |
Urgent need for mitigation, adaptation strategies, and integrated public health policies. > |
Frequently Asked Questions About Climate Change and Respiratory Health
Experts anticipate a rise in conditions such as asthma, chronic obstructive pulmonary disease (COPD) exacerbations, allergic rhinitis, and other respiratory infections. Increased air pollutants and allergens worsen these pre-existing conditions and can trigger new onset cases in vulnerable individuals.
Climate change intensifies ground-level ozone and particulate matter. These pollutants irritate airways, cause inflammation, reduce lung function, and can damage lung tissue over time. Prolonged exposure makes individuals more susceptible to infections and chronic respiratory diseases.
Yes, children, the elderly, individuals with pre-existing respiratory or cardiovascular conditions, and low-income communities are disproportionately affected. These groups often have higher exposure levels or reduced physiological capacity to cope with environmental stressors.
Individuals can monitor air quality alerts, limit outdoor activity on high-pollution days, use air purifiers indoors, wear masks when necessary, and ensure proper management of pre-existing respiratory conditions with their healthcare providers. Staying informed and proactive is key.
Urban planning can integrate green infrastructure like parks and tree planting, which help filter air pollutants and mitigate the urban heat island effect. These green spaces improve air quality, reduce temperatures, and offer health benefits, contributing to more resilient and breathable cities.
What this means
The projected 10% rise in respiratory illnesses in US cities by 2025 due to climate change is an urgent call for integrated action. This means prioritizing robust climate policies, investing in urban resilience, and strengthening public health infrastructure. Stakeholders must track ongoing air quality reports, support community-level adaptation efforts, and advocate for sustainable urban development to mitigate the escalating human cost of environmental change.